What is Idiopathic Intracranial Hypertension?
Idiopathic intracranial hypertension (IIH) means high pressure inside the skull.
Idiopathic stands for ‘unknown cause”. Intracranial means “inside the skull”, and hypertension stands for “high pressure”.
In idiopathic intracranial hypertension, the cerebrospinal fluid (CSF) that bathes the brain and spinal cord is under pressure.
In the past, the disease was named pseudotumor cerebri because the symptoms of IIH are similar to symptoms one would get with a brain tumor. Pseudotumor cerebri means “false brain tumor”.
Symptoms of Idiopathic Intracranial Hypertension
Most commonly, symptoms of IIH include headaches, blurred vision, pulsatile tinnitus, and dizziness.
Double vision, tiredness, trouble concentrating, and even depression has been reported.
Today, the term pseudotumor is outdated but some healthcare providers may still refer to this disease as pseudotumor cerebri. It is not uncommon to misdiagnose a patient with IIH as simply having a migraine headache, and be treated as such.
Diagnosing Idiopathic Intracranial Hypertension
An eye doctor can diagnose the disease during an eye exam to look at the optic nerve on the back of the eye.
The optic nerve may be swollen, which is called papilledema, and is a sign that there is increased intracranial pressure pushing against the nerve. This examination should also include a visual field test to check for subtle vision loss.
Vision loss is the most important symptom of this disease, sometimes it is only transient, when bending down or coughing, and occasionally in may be impact vision more severely. Similarly, headaches maybe worse in the morning or at night, and when bending down or lifting heavy objects.
Swelling of the optic nerve, will prompt a CT scan sometimes including dye, and/or a MRI brain scan. Those scans should also include a specific sequence to look for venous compression or stenosis of the venous outflow out of the skull. Those who have a venous compression of the venous sinus will frequently report hearing whooshing sounds or their own heartbeat. To date it is not entirely clear why some IIH patients get venous compression, and others don’t.
Finally, to confirm the disease pressure measurements will need to be obtained.
This is usually done with a spinal tap through a small needle in the lower back, and measuring the opening pressure.
The Tri-State's leaders
in Cerebrovascular treatments.
Risk Factors for Idiopathic Intracranial Hypertension
Risk factors for IIH include female gender (20-50 years old), carrying excess weight, and certain medications, steroids or high doses of vitamin A. Infections or blood clots in the veins of the brain are rarer causes.
How is Idiopathic Intracranial Hypertension Treated?
Treatment may include weight loss (though there are some people who may have this disease without being overweight).
In any case, losing weight improves the outflow of venous blood from the brain, which is why it is a very good treatment in most cases of IIH, however, it cannot be easily accomplished when also suffering from increased pressures in the skull, and the associated fatigue and frequent headaches. Patients may be put on medicine that lowers intracranial pressures (acetazolamide [Diamox®]), methazolamide, or topiramate). Those medications decrease the production of spinal fluid. Water pills (Lasix®) may be prescribed to decrease fluid retention.
It is important to realize that this disease is a long term disease, which is why patients will need more than one treatment during their life time.
Fortunately, there are several treatment options available to control the disease.
Apart from weight loss and medication, treatment may include optic nerve sheath fenestrations or rerouting excess cerebrospinal fluid from the brain or spinal cord via a thin tube to the belly. A neurosurgeon would insert those “spinal fluid shunts”.
More recently, a newer treatment method became available, a venous sinus stent. This venous sinus has nothing to do with the sinus disease over the nose, face, and forehead, rather a venous sinus is a big collecting tube in the back of the head that transports venous blood out of the brain.
Those who are diagnosed with a venous stenosis or venous compression, may qualify for a venous stent, and should be evaluated by a neuroendovascular neurosurgeon or neurologist.
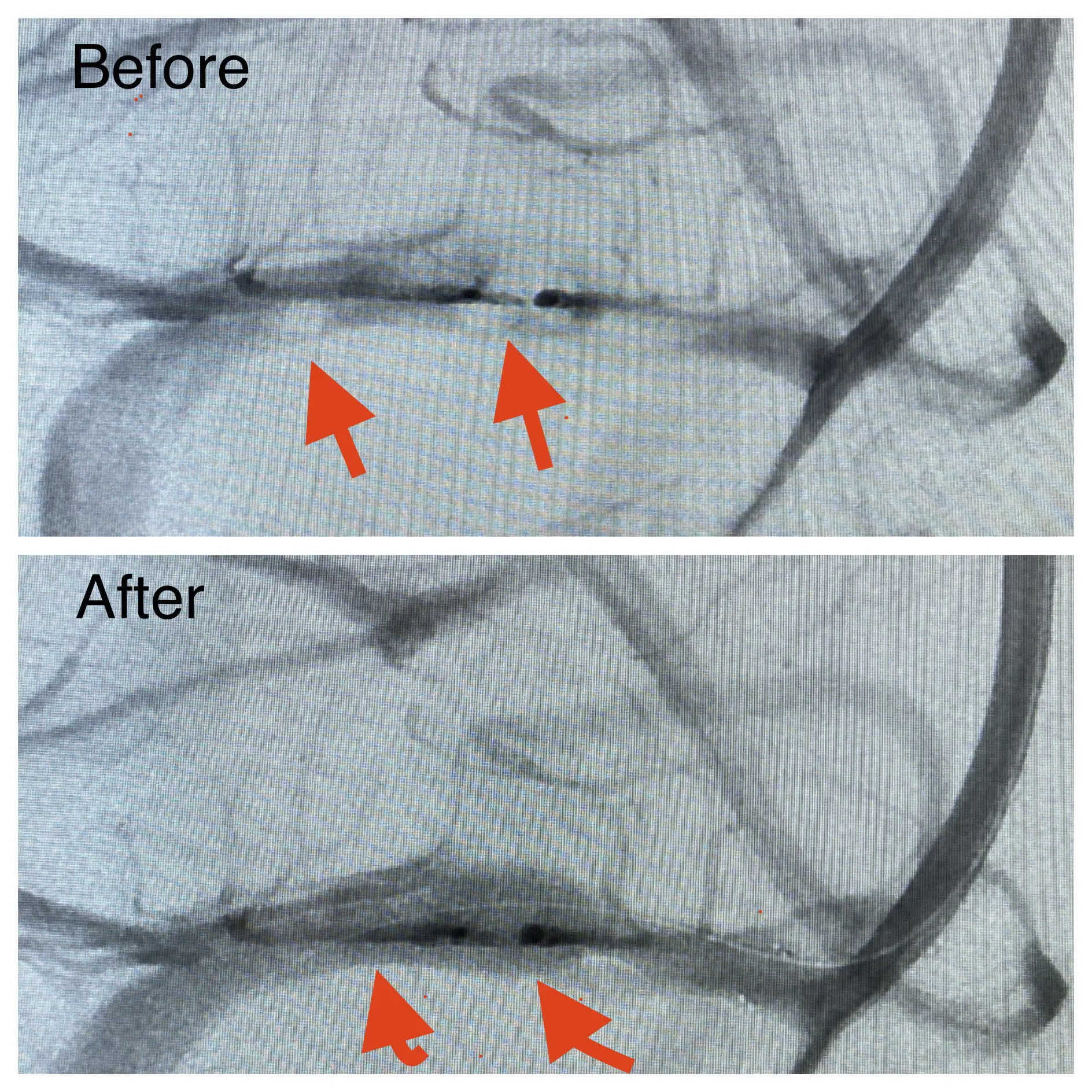
A venous stent is a wire meshed tube that can be placed through a small incision in a vein in the upper thigh by advancing a hollow tube to the venous sinus at the back of the head, using dye and specialized X-rays. A venous stent will prop open the venous compression and thereby improve the venous outflow. Venous stents are a newer kind of treatment, and the results have been very good so far, though studies are ongoing. Most patients will have immediate improvement of their symptoms, pulsatile tinnitus will be gone, and the blurry vision will improve. Headaches may improve as well.

About Dr. Dorothea Altschul
Dr. Dorothea Altschul is an accomplished neurointerventionalist in North Jersey and is the Clinical Director of Endovascular Services at Neurosurgeons of New Jersey, practicing out of their Ridgewood office located on East Ridgewood Avenue.
Recent Posts:






