Unraveling the Mysteries of Tethered Cord Syndrome
Tethered Cord Syndrome is a lesser-known condition that affects the spine. It’s not widely discussed, but it has a big impact on the lives of people who suffer from it. This condition can greatly reduce the quality of life for those affected.
This condition is often diagnosed in children but can also be found in adults. Tethered spinal cord involves the abnormal attachment of the spinal cord to the spinal column, restricting its ability to move freely.
What is Tethered Cord Syndrome?
Tethered cord syndrome is a neurological disorder characterized by an abnormal stretching of the spinal cord. It is often caused by tissue attachments that limit the movement of the spinal cord within the spinal canal. These attachments cause an abnormal stretching of the spinal cord, potentially leading to a range of symptoms and complications.
The filum terminale, a fibrous, thread-like tissue, connects the bottom of the spinal cord to the lower end of the spine. In tethered cord syndrome, this filum is often thicker and tighter than usual, causing tension on the spinal cord. This tension may be due to various factors, including a fatty mass, scar tissue from spine surgeries, or a dermal sinus tract (a narrow channel that can form a connection between the skin and deeper structures).
Tethered cord syndrome is often associated with spina bifida, a birth defect where the spinal column doesn’t close completely.
Symptoms of tethered spinal cord include:
- Lesions, hairy patches, or dimples on the lower back.
- Difficulty with bowel control.
- Lower body weakness.
- Altered gait or foot deformities.
- Back pain or scoliosis.
For adults affected by this condition, symptoms may manifest differently and can include:
- Severe pain in the lower back or legs.
- Loss of bladder or bowel control.
- Sexual dysfunction.
The presence of symptoms typically warrants further investigation, especially if they interfere with daily activities or rapidly deteriorate.
It's time to get back
to doing what you love.
Diagnosis: Beyond the Symptoms
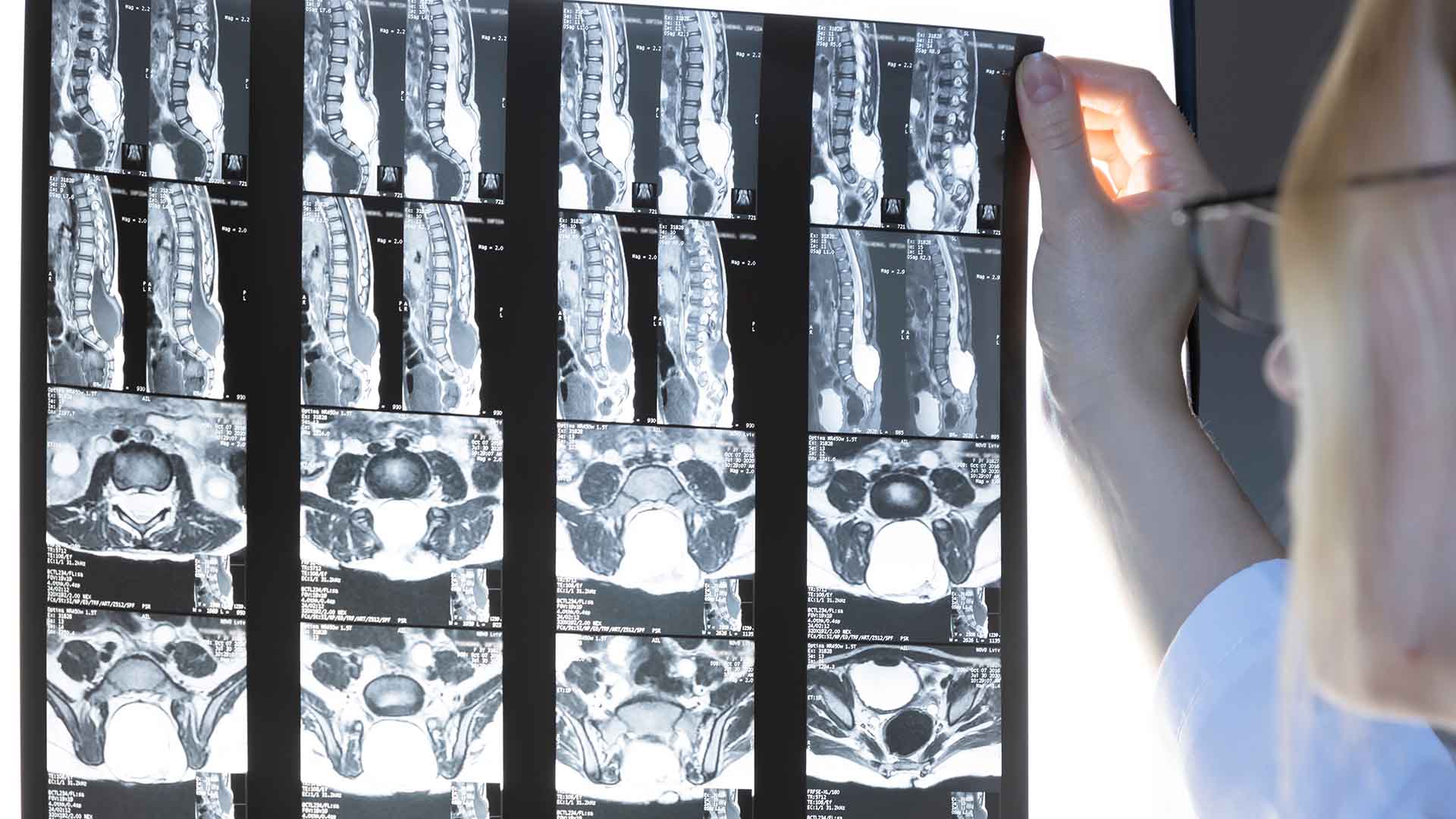
Diagnosis of a tethered cord begins with a thorough clinical evaluation, detailed patient history, and physical examination. The definitive diagnosis is usually made through imaging studies. Magnetic resonance imaging (MRI) is the gold standard for this diagnosis.
It provides clear images of the spinal cord and the structures around it, and shows if the spinal cord is abnormally stretched or showing tell-tale signs like a fatty mass or scar tissue.
Treatment Options: Releasing the Tension
When it comes to treatment for a tethered cord, the approach is often individualized, considering factors such as the patient’s age, severity of symptoms, and the degree of tethering.
- Surgical Intervention: The most common treatment is surgery to release the tethered spinal cord. This procedure involves cutting the filum terminale or removing obstructions like a tumor or fatty mass, allowing the spinal cord to hang freely. This release can prevent future neurological deterioration, although it may not eliminate existing symptoms, especially if nerve damage has already occurred.
- Conservative Management: For individuals showing no symptoms or those who might not be ideal candidates for surgery (due to other health factors), regular monitoring might be recommended. This approach includes periodic neurological evaluations and MRI scans to watch for potential progression that might necessitate surgery.
- Post-Surgical Therapies: After surgery, rehabilitation therapies, including physical and occupational therapy, may be necessary, especially if the individual has experienced muscle weakness, loss of coordination, or other neurologic issues.
Living with Tethered Cord Syndrome
Understanding that a tethered cord diagnosis is not a verdict but a condition that requires management is crucial. Post-surgery, most children and adults can return to their typical routines, albeit with some considerations for physical activities, and regular follow-up appointments are a necessity to monitor the spinal cord.
However, it’s vital to acknowledge the emotional and psychological toll that a diagnosis of tethered cord syndrome can take on patients and families. Support groups, counseling, and open communication with medical teams are invaluable components of living with this condition.
Conclusion
Tethered cord syndrome is a complex condition that calls for an informed, meticulous approach to care. Whether congenital or developed later in life due to spinal column issues like scar tissue formation from previous surgeries, recognizing the symptoms early and acting on them decisively is key.
Surgical intervention to release the spinal cord nerve, followed by comprehensive rehabilitation, offers the chance for individuals to regain much of their normal function and live fulfilling lives. Managing this condition is a lifelong process that needs constant attention and a strong support system.
If you suspect you or your loved one is experiencing symptoms of a tethered cord, seek medical attention immediately. Early diagnosis and intervention are critical in preventing additional complications and leading a healthy, active life.

About Dr. Luigi Bassani
Dr. Luigi Bassani is an accomplished board-certified neurosurgeon in Central Jersey and a proud member of Neurosurgeons of New Jersey, practicing out of their Livingston office. Dr. Bassani specializes in the diagnosis and treatment of a broad range of pediatric brain and spinal cord tumors and deformities including but not limited to pediatric epilepsy, cervical spine trauma, brain cancer, brain and skull growth abnormalities, and blood vessel disorders. In 2015 and 2017, he was named New Jersey’s Favorite Kids’ Docs for Pediatric Neurosurgery. Dr. Bassani also utilizes minimally invasive surgical techniques to treat adult patients suffering from brain tumors, herniated discs, and spinal trauma or degeneration. He’s accepting new patients.
Recent Posts: