General Overview
Cervical disc replacement surgery, aka cervical arthroplasty, has become an effective treatment option for patients suffering from symptoms due to degenerative disc disease of the cervical spine.
Unlike fusion surgery, the artificial disc replacement maintains motion between the vertebrae 1.
What is Artificial Disc Replacement?
The cervical artificial disc is a mechanical device that is meant to imitate the range of motion allowed by the intervertebral disc, the cartilage cushion between the vertebrae of the cervical spine.
Patients who require spine surgery for complaints due to degenerative disc disease of the neck have traditionally been treated with an anterior cervical discectomy and fusion (ACDF). The goal of this operation is to remove bone spurs and damaged disc material that compress the spinal cord and spinal nerves. The space created is filled with a bone graft that allows growth of bone to occur between the vertebrae, aka the fusion. The downside of fusion surgery is that neck motion is eliminated.
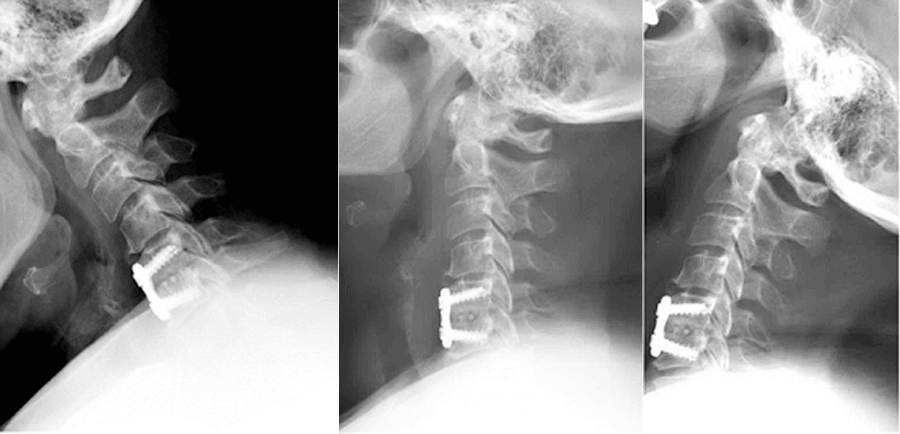
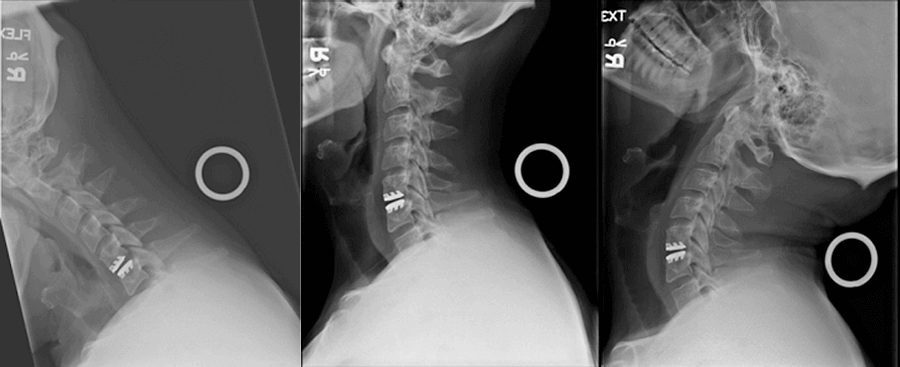
Patient with a cervical fusion – motion eliminated between the 5 th and 6 th cervical vertebrae
Cervical disc replacement surgery avoids the negative consequences of a fusion, including the possibility of neck pain if the bones fail to heal. Another drawback of a fusion is a condition known as adjacent segment disease, degeneration of normal areas of the spine due to increased pressure created by the fusion 2.
A clear advantage of receiving a cervical artificial disc is that patients are able to resume their normal activities much sooner since no bone healing required. The device is designed to provide immediate support for normal neck mobility and stability.
Who is a candidate for Artificial Disc Replacement?
Degeneration of the cervical spine leads to formation of bone spurs and possibly a herniated disc.
This narrowing is known as spinal stenosis and puts pressure on the spinal cord and spinal nerves, leading to a “pinched nerve”. Patients may experience a variety of complaints due to these degenerative changes including neck pain, arm pain, numbness, and or weakness. Patients who do not respond to conservative treatment or patients presenting with serious numbness/weakness may require surgery 3.
Consultation with an experienced spine surgeon is necessary to receive the appropriate medical advice. Not every patient is candidate for a cervical artificial disc. A thorough neurological exam and evaluation of the patient’s imaging is required to determine if cervical disc replacement surgery is the right choice.
How is an Artificial Disc Replacement performed?
The operation is similar to an anterior cervical discectomy and fusion, however instead of the bone graft, the cervical artificial disc is inserted.
The procedure is performed under general anesthesia. A skin incision is made in the front of the neck. The neck structures are separated by gentle dissection to access the cervical spine.
An X-ray is obtained to confirm that the appropriate area in the neck has been exposed. The degenerated disc and bone spurs are removed, this is known as the discectomy. The discectomy creates a wider nerve channel and relieves pressure on the spinal cord and nerve roots. The release of the nerves allows recovery of neurological function and improvement in the arm pain and/or numbness and weakness. In order to maintain stability of the spine, however the space previously occupied by the damaged disc needs to be supported.
Once the disc space has been cleaned out, a cervical artificial disc is inserted. Precise positioning of the device is required in order for proper function. Successful implantation is checked with X-rays. Improvement in neck pain occurs due to the replacement of the worn-out disc with the artificial disc. The incision is closed with a single suture that is under the skin.
What is it like after surgery?
Following the operation, patients will experience some swallowing discomfort and may require softer foods for one or two weeks.
There is usually minimal pain at the incision site. Unlike fusion surgery, there is no necessity to limit range of motion, so patients do not need to wear an uncomfortable collar. In a relatively short time, patients can resume their normal activities. After surgery, patients are followed with periodic X-rays to make sure the artificial cervical disc is working appropriately.
Summary
Cervical disc replacement surgery is a highly successful operation when performed for the appropriate indications
Patients can appreciate significant improvement in their quality of life. A comprehensive evaluation by an experienced spine surgeon is necessary to make sure artificial disc replacement is the correct surgical option.
Citations
- Roberts, T.T., et al., Cervical Total Disk Arthroplasty. Clin Spine Surg, 2018. 31(1): p. 6-13.
- Tobert, D.G., et al., Adjacent Segment Disease in the Cervical and Lumbar Spine. Clin Spine Surg, 2017. 30(3): p. 94-101.
- Kaiser, M.G., Multilevel cervical spondylosis. Neurosurg Clin N Am, 2006. 17(3): p. 263-75, vi.

About Dr. Michael G. Kaiser
Dr. Michael G. Kaiser is a nationally recognized neurosurgeon in North Jersey and is a proud member of Neurosurgeons of New Jersey, practicing out of their Ridgewood office conveniently located on East Ridgewood Avenue. Dr. Kaiser specializes in complex and minimally invasive spine surgeries.
Please call today to schedule a consultation with me.
(551) 284-3265
Request a consultation with Dr. Kaiser

