What is a lumbar puncture?
Lumbar puncture, also known as a spinal tap, can be used as a diagnostic tool for idiopathic intracranial hypertension (IIH), previously known a pseudotumor cerebri. IIH is a condition characterized by increased pressures within the skull without an identifiable cause. It primarily affects young overweight women, but it can occur in individuals of any age or gender. IIH can cause headaches, pulsatile tinnitus, occasional blurry vision, or vision loss.
What is a lumbar puncture used for?
Lumbar puncture is just one component of the diagnostic process for IIH and is used to assess CSF pressure and exclude other possible causes.
In the case of IIH, the CSF pressure is typically elevated. By measuring the opening pressure and analyzing the composition of the CSF, a lumbar puncture can help in the diagnosis of IIH and in ruling out other potential causes of increased intracranial pressure, such as infection or tumor.
In addition to measuring the opening pressure, the CSF obtained during a lumbar puncture can be send for further testing, including cell count, protein levels, glucose levels, and microbiological cultures. These tests help in evaluation the underlying cause of increased intracranial pressure and ruling out other conditions.
How is a lumbar puncture done?
During a lumbar puncture, a thin needle is inserted into the lower back, into the fluid filled space surrounding the spinal cord. This allows for the collection of cerebrospinal fluid (CSF), the fluid that surrounds the brain and spinal cord.
The procedure typically involves the patient lying on their side with their back curved forward. It can be also done in the sitting position hunched over but it is less preferred for IIH patients due to inaccurate assessment of intracranial pressures.
A local anesthetic is injected into the skin and deeper tissues to numb the area. A needle is carefully inserted between the lumbar vertebrae, usually between L3 and L4, or L4 and L5. Once the needle is in place, a small tube is connected which measures the pressure. Then, the CSF is collected by allowing it to drip into collection tubes.
After collecting the necessary amount of CSF, the needle is gently removed, and a sterile dressing is applied to the puncture site.
Is lumbar puncture safe?
Lumbar puncture is generally considered safe, but like any medical procedure, it carries some risks, including: discomfort or pain during the procedure, headache, which is the most common side effect but usually resolves within a few days. Infection, although rare, can occur if proper sterile techniques are not followed. Bleeding or bruising at the puncture site can also occur. Rarely, more serious complications can occur, such as nerve damage, spinal cord injury, or brain herniation, but these are extremely rare.
After the procedure, the patient is typically asked to lie flat for a minimum of one hour to minimize the risk of post-spinal tap headache. It is advised to stay well hydrated, and to avoid strenuous activities for a day or two.
Occasionally, a lumbar puncture cannot be performed safely with the technique described above. If due to scaring tissue, prior surgeries, or other anatomical reasons, the appropriate amount of spinal fluid cannot be obtained, other options exist.
There is a possibility to obtain a lumbar puncture in a specialized procedure room utilizing continuous X-ray called fluoroscopy. Same risks and after care applies to a lumbar puncture under fluoroscopy, and it takes trained medical professionals to perform those type of procedures under appropriate circumstances. The procedure is tailored to each patient’s specific needs, and the information provided here is a general overview.
It is important to note that lumbar puncture is not the sole diagnostic tool for IIH. Diagnosis is made based on a combination of clinical presentation, neurological examination findings, imaging studies (such as magnetic resonance imaging or computed tomography), and ruling out other potential causes. A visit to the eye doctor is typically involved as well to assess for an enlarged blind spot and swelling of the optic nerve. That is best evaluated by dilating the pupil and looking at the back of the eye.
The Tri-State's leaders
in Cerebrovascular treatments.
Lumbar puncture is just one component of the diagnostic process for IIH and is particularly helpful when a high volume tap needs to be performed to remove CSF. High volume taps may be needed for immediate relief of symptoms.
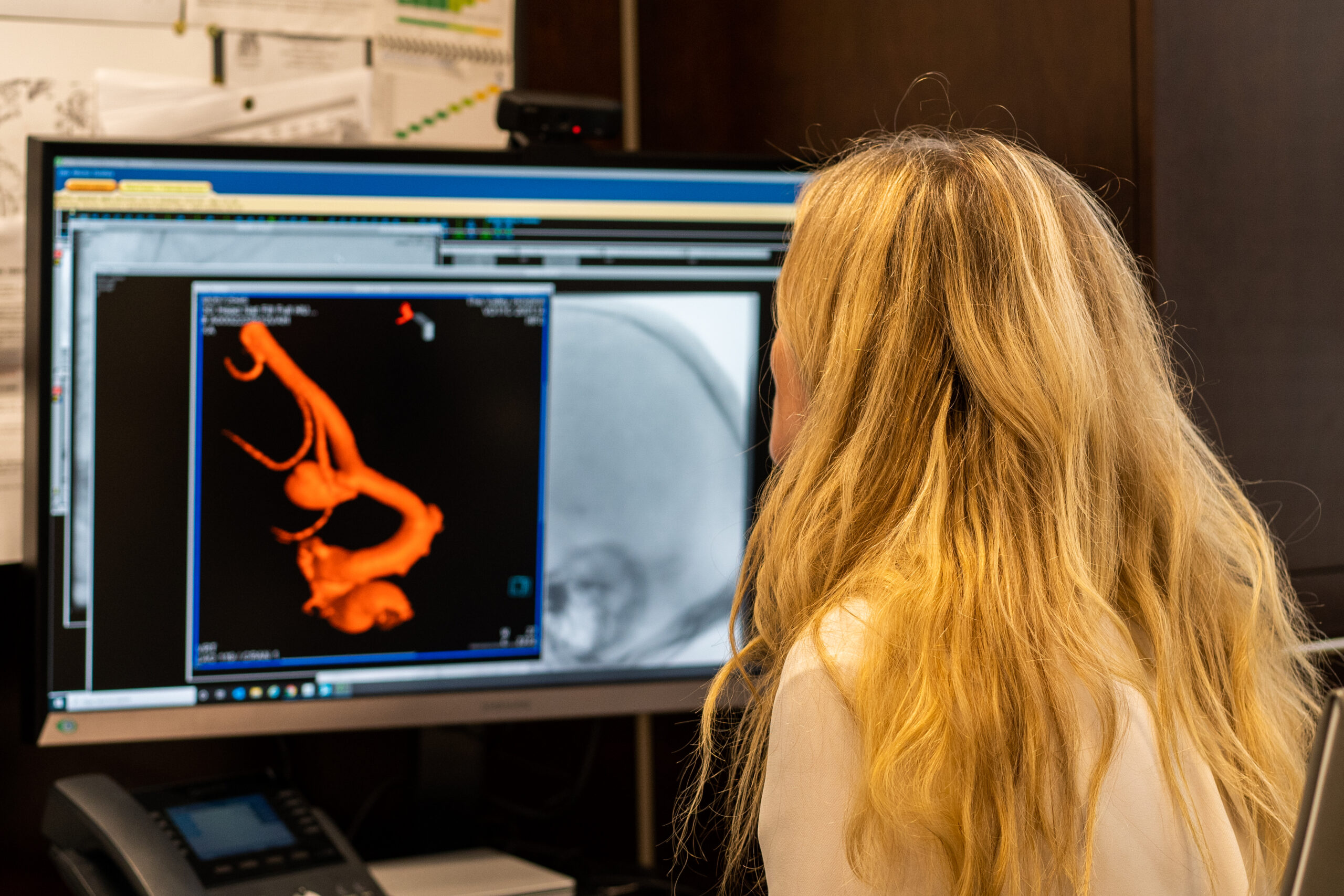
Intracranial pressure measurements can also be obtained during a cerebral angiogram (refer to other blog). For patients with venous stenosis and IIH, venous pressures can be obtained, by inserting a small hollow tube into the vein through a small incision in the groin.
The insertion site is numbed with a local anesthetic to minimize discomfort. A thin, flexible catheter is inserted into the target vein under sterile conditions. The catheter is advanced to the desired location using continuous X-rays, called fluoroscopy, using a specialized imaging machine.
Once the catheter is correctly positioned, the pressure within the vein is measured and recorded using a pressure transducer connected to the catheter. The pressure readings can be visualized on a monitor and recorded for further analysis.
Multiple areas in the brain and neck are used to record the pressures. A total cranial gradient is calculated. That gradient can be increased in most IIH patients.
Those measurements are helpful in evaluating IIH patients, and it aids in identifying the site and severity of venous blockages (stenosis) or compressions. Those with a venous compressions may benefit from venous sinus stenting.
Patients who hear their own pulse may have IIH, and hearing one’s own pulse is often associated with a venous compression. (refer to blog on hearing your own pulse) https://www.neurosurgeonsofnewjersey.com/blog/are-you-hearing-your-heartbeat-in-your-ear/ Other treatment methods for IIH involve weight loss, medication, and other surgical CSF diversion techniques.

About Dr. Dorothea Altschul
Dr. Dorothea Altschul is an accomplished neurointerventionalist in North Jersey and is the Clinical Director of Endovascular Services at Neurosurgeons of New Jersey, practicing out of their Ridgewood office located on East Ridgewood Avenue.
Recent Posts: