Understanding Herniated Disc: An Overview
What is a herniated disc?
A herniated disc, also called slipped disk, can cause back and neck pain, numbness, weakness, and difficulty walking.
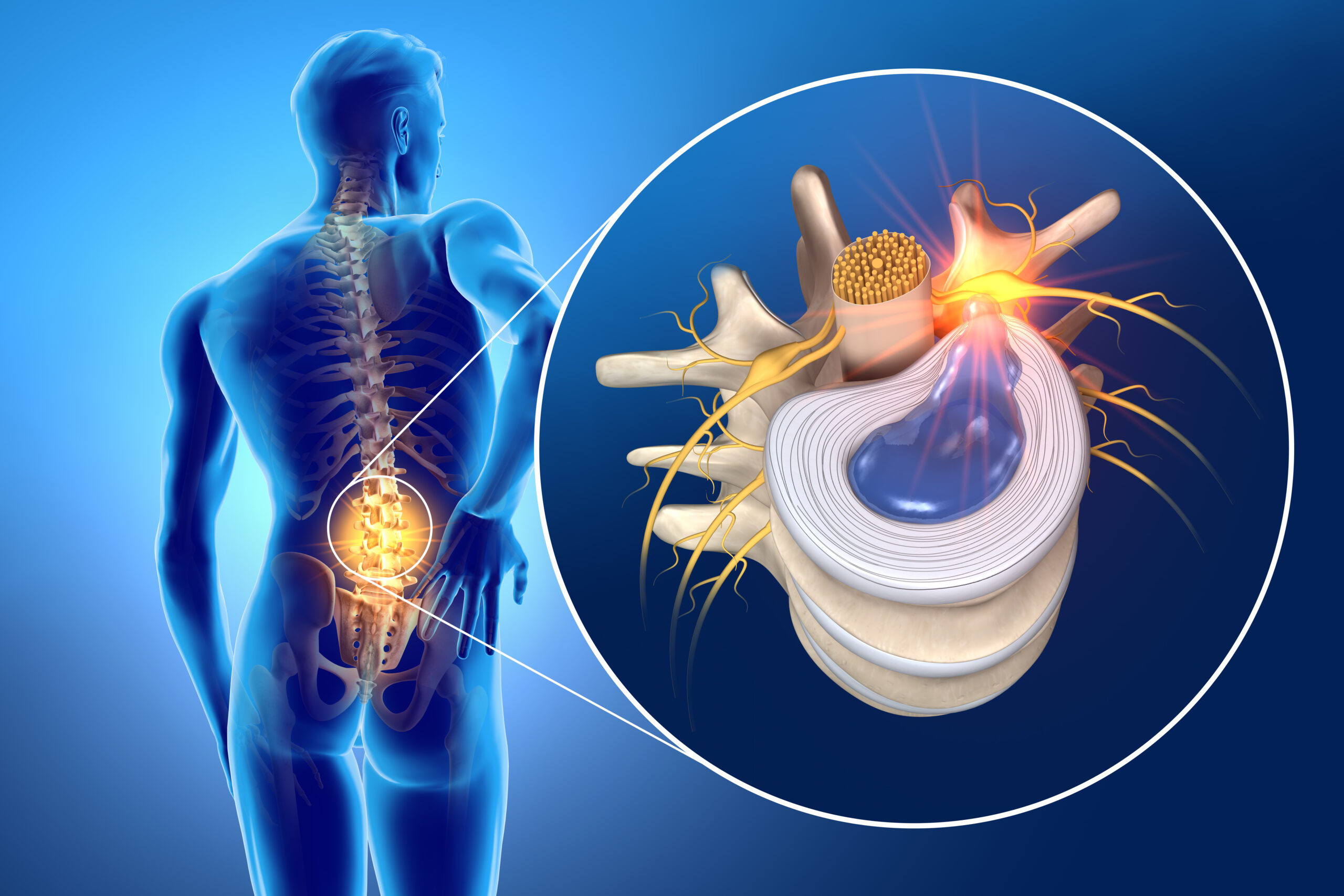
This condition refers to a problem with the cushions that separate the bones in your spine. These cushions called discs, act as shock absorbers to provide cushioning and flexibility to your spinal cord.
Now, imagine a disc as a jelly-filled doughnut. The outer part of the disc is tough, like the doughnut’s crust, and the inside is soft and jelly-like. When the gel inside the disc (called the nucleus pulposus) leaks out due to a crack or tear, it causes a herniated disk.
When this happens, the herniation can put pressure on nearby spinal nerves causing pain, numbness or weakness. You may also have neck or back pain depending on the affected part of the spine.
Preventing Herniated Discs
While certain risk factors for herniated discs, such as age and genetics, cannot be changed, there are preventive measures individuals can take to reduce the risk of developing this condition:
Maintain a Healthy Weight:
Excess weight puts additional stress on the spine, increasing the likelihood of disc herniation. Maintaining a healthy weight through a balanced diet and regular exercise can help alleviate this stress.
Practice Good Posture and Ergonomics:
Maintaining proper posture while sitting, standing, and lifting heavy objects can reduce strain on the spine and minimize the risk of disc herniation. Using ergonomic techniques, such as adjusting chair and desk heights or using proper lifting techniques, can also help prevent spinal injuries.
Engage in Regular Exercise and Strengthening Activities:
Regular exercise, including activities that promote core strength and flexibility, can help support the spine and reduce the risk of disc herniation. Exercises such as walking, swimming, yoga, and Pilates can be beneficial.
Lift Objects Properly:
When lifting heavy objects, it is important to use the proper lifting technique. Bend your knees, keep your back straight, and lift with your legs rather than your back to minimize strain on the spinal discs.
Causes of herniated discs
Herniated discs can happen due to different reasons like aging, spine injury, repetitive stress, bad posture, and genetics. Age-related wear and tear on the spinal discs is a common cause of disc herniation.
As we age, the spinal discs lose some of their water content, making them less flexible and more prone to herniation. Trauma or injury to the spine, such as from a fall or lifting heavy objects incorrectly, can also cause discs to herniate.
Engaging in activities that require frequent bending, lifting, or twisting, particularly with poor body posture, can strain the spinal discs. This strain increases the likelihood of developing a hernia.
Furthermore, individuals with a family history of herniated discs may have a higher chance of developing this condition.
Lower back (lumbar spine)
If the herniated disk is in the lower back, the pain often affects the buttocks, thighs, and calves. Pain travels along the path of the sciatic nerve, from the buttock, down the legs. This leg pain is known as sciatica.
Neck (cervical spine)
If the issue occurs in the neck, pain and weakness are more likely to be present in the shoulders and arms.
Middle back (Thoracic Spine)
A herniated disk in the middle of the back is likely to cause pain around the location of the herniation. Pain may travel around the rib cage to the front of the body. This is not as commonly seen as herniations of the lumbar and cervical spine
It's time to get back
to doing what you love.
Symptoms of Herniated Discs
A symptom of back or neck pain is common and may vary depending on the location and severity of the herniation.
- Numbness or tingling: This can happen when a herniated disk presses on the spinal cord or the nearby nerves that exit the spinal canal. The sensations may travel outwards along the nerve roots into the arms or legs.
- Muscle weakness: When a herniated disk presses on a nerve, the muscle strength may be reduced causing problems with walking.
- Pain: Pain usually occurs in the back and may radiate out to the arms or legs. People sometimes describe the pain as sharp or burning.
A severely herniated disk in any region of the back can potentially cause loss of bladder or bowel control. If a person has back pain and changes to their bladder or bowel control they should seek emergency medical attention.
Diagnosis
To diagnose a herniated disc, your doctor will usually perform a thorough physical examination and review your medical history.
Your doctor may also order imaging tests like MRI or CT scans to confirm the diagnosis and check how serious the condition is.
Herniated Disc Treatment
There are many conservative treatments options available for people suffering from this condition.
Most patients with disc herniations do not need surgery. Most herniated discs heal on their own with conservative treatment and time.
Depending on how severe the herniation, your health care provider may suggest less invasive treatments. Some of these include:
- Rest and activity modification: Adequate rest and avoiding activities that exacerbate symptoms are recommended to allow the body to heal.
- Pain management: Over-the-counter pain relievers, such as nonsteroidal anti-inflammatory drugs (NSAIDs), may be used to alleviate pain and reduce inflammation.
- Muscle relaxants: These medications can help relieve muscle spasms associated with a herniated disc.
- Physical therapy: Physical therapy plays a crucial role in herniated disc treatment. It involves exercises, stretches, and other therapeutic techniques to strengthen the surrounding muscles, improve flexibility, and reduce pain.
If your condition is severe and less invasive options haven’t worked, you and your doctor can talk about surgery.
Surgery for Herniated Discs
The most common surgical procedures used to alleviate herniated discs are:
- Microdiscectomy: This procedure is usually done in less severe cases. Surgeons remove pieces of the disc to take pressure off of the affected nerves.
- Artificial Disc Replacement: Surgeons completely remove the disc and replace it with an artificial disc. This mimics the movement of our natural discs.
- Fusion: Surgeons remove the herniated disc, then fuse the vertebrae on either side of where the herniated disc was, essentially creating one longer vertebra.
Recovery time varies depending on the surgical procedure performed, the person’s overall health, and the extent of the herniation.
In many cases, herniated discs heal on their own with conservative treatment and time. The body’s natural healing processes, along with proper care and lifestyle modifications, can lead to symptom improvement and disc healing.
This article provides a brief overview, but please note that each person’s situation is unique. It is essential to consult with a qualified healthcare professional for a comprehensive evaluation and personalized advice regarding herniated discs.
Don’t suffer with the pain of herniated discs any longer! Contact our office today to schedule a consultation with one of our board-certified physicians.

About Dr. Christopher Gillis
Dr. Christopher Gillis is an accomplished neurosurgeon in Central Jersey and a proud member of Neurosurgeons of New Jersey, practicing out of their West Long Branch office conveniently located on Highway 36 West. Dr. Gillis is a fellowship trained spine surgeon out of Rush University in Chicago and his specialty is minimally invasive and complex brain and spine surgery. His clinical and research interests include developing and advancing innovative techniques for minimally invasive spine surgery, spine deformity correction, revision spine surgery, as well as robotics. Dr. Gillis’ passion is driven by helping patients regain their quality of life after suffering from disabling medical conditions. He is currently accepting new patients.
Recent Posts: