General Overview
Irritation or injury of the spinal cord within a patient’s neck, the cervical spine, is known as Cervical Myelopathy.
The most common cause is degenerative disc disease, aka spondylosis, leading to the condition known as cervical spondylotic myelopathy 1.
What is Cervical Spondylotic Myelopathy?
The neck is made up of seven bones called vertebrae. The vertebrae are separated by the discs which act as a cushion. Each pair of vertebrae are also connected by two joints along the back of the spine, known as the facet joints.
The surrounding ligaments, like the posterior longitudinal ligament, help to hold secure the vertebrae. Working together, these structures allow normal movement of the cervical spine 2.
As we get older, wear and tear of the spine causes the discs to deteriorate. The outer wall of the disc weakens, leading to collapse and escape of the internal contents, a herniated disc. Bone spurs form as the surrounding ligaments, like the posterior longitudinal ligament, are separated from the vertebrae.
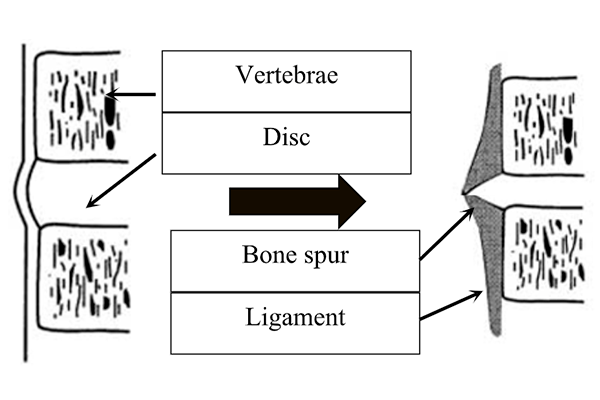
Bone Spur Formation
This results in abnormal motion that places increased pressure on the facet joints and the development of more bone spurs. As time goes on, an abnormal, tipping forward of the cervical spine develops, known as a kyphosis 3.
Patients can develop neck pain since these joints are no longer working properly. More concerning is the development of cervical spinal stenosis, narrowing of the spinal canal that contains the spinal cord and nerve roots. The narrowing puts pressure on the spinal cord and leads to myelopathy. Pressure on the nerve roots will cause more specific complaints in one or both arms, known as a radiculopathy.
Patients developing symptoms of cervical myelopathy will typically describe:
- hand tingling and numbness
- loss of fine motor skills or hand coordination
- arm and/or leg weakness
- balance problems or trouble walking
- difficulty with urination
- possible neck pain and stiffness
It is important to remember that the presence of neck pain alone is not indicative of a cervical myelopathy. In fact, many patients with cervical spondylotic myelopathy have no neck pain. The natural history of cervical spondylotic myelopathy is variable. Patients can present with stable complaints or demonstrate a progressive decline 4. Therefore, patients presenting with neck issues should be evaluated by an experienced spine specialist.
How is Cervical Spondylotic Myelopathy diagnosed?
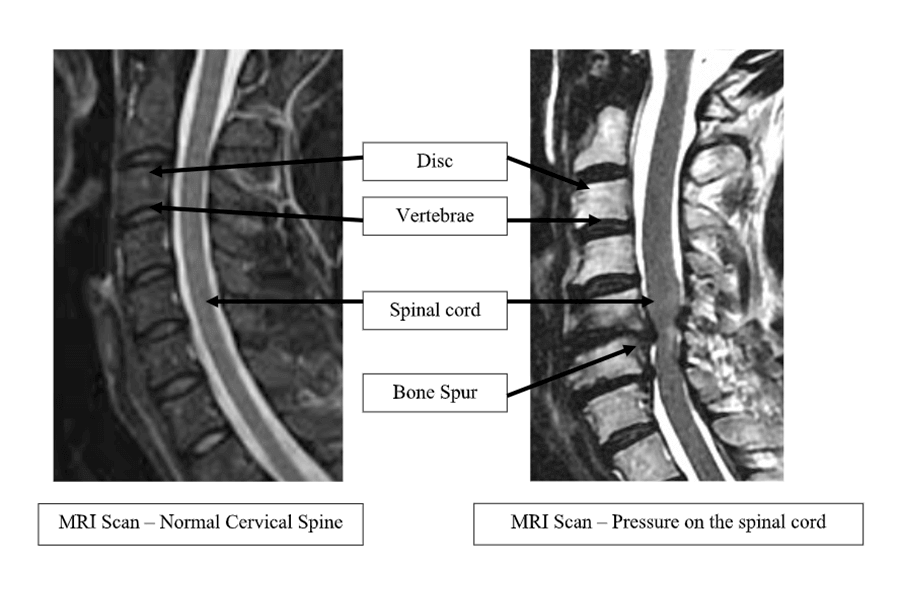
The diagnosis of cervical spondylotic myelopathy is dependent on the physical examination, neurological assessment, and review of imaging.
X-rays are obtained to evaluate the shape of the cervical spine and determine if there is any abnormal movement. More advanced imaging is required to assess the spinal cord and nerve roots. A CT (computed tomography) provides valuable information regarding the size of the spinal canal and bone structure. An MRI (magnetic resonance imaging) scan is the best study to demonstrate pressure on the spinal cord and nerve roots 5.
What Treatments are available?
Conservative treatment may be an option for a patient with cervical spondylotic myelopathy.
Observation, physical therapy, and pain treatments may be useful if neck pain is the primary complaint, or the symptoms of cervical myelopathy are mild and/or stable. Physical therapy is intended to reduce neck pain, improve posture, and help reverse or stabilize weakness. Fine motor skills may improve with focused exercises to improve hand coordination and gait problems.
Surgical treatment is recommended for patients who do not respond to conservative treatment or present with significant or progressive loss of function. Each patient requires an individualized surgical plan, using the information from the physical examination and imaging 6. There are a number of acceptable surgical treatment options including:
- Anterior cervical discectomy and fusion
- Anterior cervical corpectomy and fusion
- Posterior Cervical laminectomy with or without fusion
- Posterior Cervical laminoplasty
These operations are performed under general anesthesia. Surgery is intended to widen the spinal canal and relieve pressure on the spinal cord and nerve roots. The incision can be made in the front of the neck, anterior procedures, or the back of the neck, posterior approaches. With certain procedures the removal of a herniated disc or bone spurs can lead to spinal instability.
To prevent neck pain or development of a deformity, a fusion operation may be included. The goal of a spinal fusion is to secure the spine and have bones heal together. The fusion is accomplished through the implantation of bone graft and metallic devices, such as metal plates and screws. Immediate stability is provided by the metal implants and long-term security through healing of the bones.
The decision to pursue surgery, requires careful consideration of all the available data. Surgery should not be recommended based only on the results of an MRI scan. The mere presence of cervical spinal stenosis does not justify surgery. The patient’s presentation and symptoms need to match the findings of their imaging. Consultation with an experienced spine specialist is necessary.
What is the Prognosis of Cervical Spondylotic Myelopathy?
The patient with cervical spondylotic myelopathy has the opportunity to improve after treatment.
In general, there are three factors that help predict the outcome of treatment:
- The severity of cervical myelopathy symptoms
- The duration of the symptoms of cervical myelopathy
- How fast did symptoms develop?
To improve treatment response, the diagnosis of cervical myelopathy should be made as soon as possible. This is particularly important if symptoms of cervical myelopathy are progressing. The sooner the patient is treated, the more likely improvement will be appreciated 7.
Summary
Cervical Spondylotic Myelopathy is a condition where degenerative changes of the cervical spine cause spinal cord irritation and/or injury.
Patients typically present with complaints of weakness, sensory changes, and possibly neck pain. A thorough physical examination and evaluation of imaging, such as an MRI scan, is required to make the diagnosis.
Although conservative treatment may be an option, for severe or progressive symptoms of cervical myelopathy, surgical treatment is preferred. Consultation with an experience spine surgeon will avoid treatment delay and provide the best opportunity for recovery.
Citations
- Lyer A, Azad TD, Tharin S. Cervical Spondylotic Myelopathy. Clin Spine Surg 2016 Dec;29(10):408-414. doi: 10.1097/BSD.0000000000000397.
- Louis-Ugbo J, Pedlow Jr. FX, Heller JG. (2012) Antomy, Biomechanics, and Clinical Implications. In Benzel EC (Ed.) The Cervical Spine, 5th (1-33). Lippincott Williams & Wilkins: Philadelphia.
- Shedid D, Benzel EC. Cervical spondylosis anatomy: pathophysiology and biomechanics. Neurosurgery2007 Jan:60(supp1):S7-13. Doi: 10.1227/01.NEU.0000215430.86569.C4.
- Matz PG, Anderson PA, Holly LT, Groff MW, Heary RF, Kaiser MG, Mummaneni PV, Ryken TC, Choudhri TF, Vresilovic EJ, Resnick DK; Joint Section on Disorders of the Spine and Peripheral Nerves of the American Association of Neurological Surgeons and Congress of Neurological Surgeons. The natural history of cervical sponyloltic myelopathy. J Neurosurg Spine. 2009 Aug;11(2):104-11. doi: 10.3171/2009.1.SPINE08716.PMID: 19769489
- Bakhsheshian J, Mehta VA, Liu JC. Current Diagnosis and Management of Cervical Spondylotic Myelopathy. Global Spine J. 2017 Sep;7(6):572-586. doi: 10.1177/2192568217699208. Epub 2017 May 31.
- Kaiser MG. Multilevel cervical spondylosis. Neurosurg Clin N AM. 2006 Jul;17(3):263-75, vi. doi: 10.1016/j.nec.2006.04.008
- Holly LT, Matz PG, Anderson PA, Groff MW, Heary RF, Kaiser MG, Mummaneni PV, Ryken TC, Choudhri TF, Vresilovic EJ, Resnick DK; Joint Section on Disorders of the Spine and Peripheral Nerves of the American Association of Neurological Surgeons and Congress of Neurological Surgeons. Clinical prognostic indicators of surgical outcome in cervical spondylotic myelopathy. J Neurosurg Spine. 2009Aug:11(2):112-8. Doi: 10.3171/2009.1.SPINE08718.

About Dr. Michael G. Kaiser
Dr. Michael G. Kaiser is a nationally recognized neurosurgeon in North Jersey and is a proud member of Neurosurgeons of New Jersey, practicing out of their Ridgewood office conveniently located on East Ridgewood Avenue. Dr. Kaiser specializes in complex and minimally invasive spine surgeries.
Please call today to schedule a consultation with me.
(551) 284-3265
Request a consultation with Dr. Kaiser

